Consensus statement on the role of health systems in advancing the long-term well-being of people living with HIV
There have been substantial reductions in AIDS-related illness and deaths since the introduction of antiretroviral therapy (ART) in 1996. By the end of 2019, 67% of people living with HIV had started treatment with ART and 59% had achieved viral suppression. Despite access to effective ART and viral suppression, people living with HIV often report poor well-being and health-related quality of life.
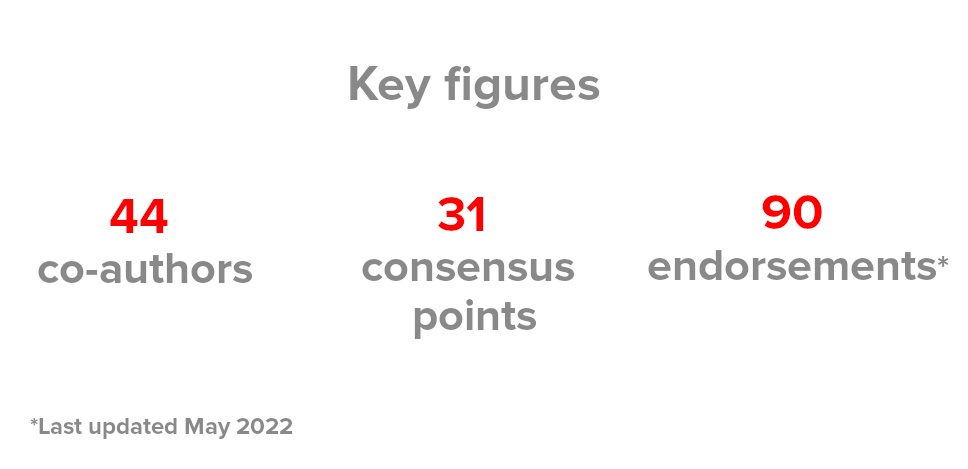
A multidisciplinary panel of 44 global HIV experts articulate how health systems can advance the long-term well-being of people living with HIV by addressing multimorbidity, health-related quality of life, stigma and discrimination using an holistic and patient-centred approach. The 31 consensus points presented in “Consensus statement on the role of health systems in advancing the long-term well-being of people living with HIV” have been endorsed by 90 organisations and counting by May 2022 (see the list with endorsements below).
This project was led by HIV Outcomes Co-Chair and professor at the Barcelona Institute for Global Health (ISGlobal) Dr Jeffrey V. Lazarus and co-chaired by Ricardo Baptista-Leite (UNITE Founder and President), Nikos Dedes (HIV Outcomes Co-Chair), and Adeeba Kamarulzaman (IAS President). In addition to the co-chairs, the Steering Committee members included Jane Anderson (HIV Outcomes Co-Chair), Georg Behrens (HIV Outcomes Steering Group Member and EACS Medical Secretariat Guidelines Chair), Georgina Caswell (GNP+ Head of Programmes), María José Fuster-Ruiz de Apodaca (SEISIDA Director and HIV Outcomes General Member), Prof Richard Harding (HIV Outcomes General Member), Dr Caroline Sabin (HIV Outcomes General Member), and Kelly Safreed-Harmon (HIV Outcomes General Member).
Read the full text of the Consensus Statement Endorse the Consensus Points
Consensus points on the role of health systems in advancing the long-term well-being of people living with HIV (PLHIV)
Framing a more comprehensive health agenda for people living with HIV (PLHIV)
1.1. PLHIV at all stages of their lives face unique health challenges. Therefore, health systems need to provide comprehensive healthcare for PLHIV and focus on additional outcomes beyond virological suppression.
1.2. The World Health Organization’s definition of health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” as well as the Sustainable Development Goal of “[ensuring] healthy lives and [promoting] well-being for all at all ages” underscores the need for healthcare paradigms that look beyond HIV-focused care to address the overall health and well-being of PLHIV in an integrated, people-centred manner.
1.3. New clinical and public health targets are needed in all countries, regardless of economic status, in order to optimise health system resources, achieve better health engagement, and improve health outcomes in PLHIV.
1.4. Respecting, protecting and fulfilling human rights is a necessary element of a strong, effective response to HIV, and this approach should be embodied in all efforts to address the long-term health needs of PLHIV. This approach encompasses attention to service delivery, structural inequalities, and laws, policies and practices that affect the health and well-being of PLHIV.
1.5. Actions to advance the health of PLHIV should be equitable, with consideration of the disproportionate burden of HIV among key populations and of the intersectional nature of the stigma and discrimination experienced by many members of these populations.
1.6 Efforts to improve healthcare for PLHIV should be aligned with efforts to expand universal health coverage in accordance with the 2019 United Nations Political Declaration on Universal Health Coverage and related global commitments.
1.7. In accordance with the Greater Involvement of People Living with HIV (GIPA) Principle and the World Health Organization Framework on Integrated People-Centred Health Services, PLHIV should be meaningfully involved in the planning, implementation and monitoring of all interventions to safeguard and improve their health.
Multimorbidity
2.1. Both biological and non-biological factors put PLHIV at higher risk than people without HIV for a range of health concerns, including infectious and noncommunicable diseases, resulting in a greater multimorbidity burden in PLHIV.
2.2. Mental health comorbidities are highly prevalent among PLHIV worldwide, along with physical health comorbidities. They both warrant urgent attention from policy-makers and service providers.
2.3. Integrated approaches to multimorbidity prevention and management can reduce current health system inefficiencies and facilitate greater engagement and retention in care.
2.4. Addressing multimorbidity as a component of comprehensive long-term care for PLHIV entails considering issues reported by PLHIV to undermine their health-related quality of life (HRQoL), such as pain, fatigue, sleep disturbance, and episodic and chronic disability.
2.5. Integrated, evidence-based, people-centred models of care for the prevention and management of multiple conditions in PLHIV should provide multidisciplinary team care and effective referral to psychosocial health services.
2.6. Global monitoring of national HIV responses with regard to comorbidities should include the collection and reporting of disaggregated data for a range of infectious and noncommunicable diseases.
2.7. In their HIV monitoring activities, national health systems should include not only comorbidities specified in global HIV monitoring, but also other comorbidities that are relevant to their particular national contexts.
2.8. Causes of mortality among PLHIV should be monitored at the national level using uniform coding for comparative purposes.
2.9. Health system data on patterns of morbidity and causes of mortality in PLHIV should be published and used to guide nationally targeted efforts to improve multimorbidity prevention and care in this population.
Self-reported health-related quality of life (HRQoL)
3.1. HRQoL is a central aspect of long-term health and well-being. Improving the HRQoL of PLHIV has the potential to improve various outcomes including medication adherence, retention in care, and ultimately clinical outcomes.
3.2. The effectiveness of healthcare for PLHIV should be assessed using more than biomedical outcomes. Self-reported HRQoL should be recognised as a core outcome in the clinical management of individual patients as well as in national and global monitoring of health system responses to HIV.
3.3. The use of patient-reported outcome measures (PROMs) in clinical care for PLHIV has a number of potential benefits, including achieving a person-centred approach; using health system resources more efficiently; empowering PLHIV to raise concerns; facilitating discussion of sensitive problems; encouraging greater engagement with services; and promoting treatment adherence.
3.4. Validated HIV-specific PROMs should be used to measure the HRQoL of PLHIV in clinical practice, with findings informing efforts to address issues that are reported to be undermining HRQoL.
3.5. Health system monitoring of HRQoL should use both HIV-specific and non-HIV-specific validated PROMs, with the latter enabling comparisons of the HRQoL of PLHIV to that of people without HIV.
3.6. HRQoL outcomes in PLHIV may be influenced by multifactorial causal pathways involving diverse issues such as multimorbidity, frailty, symptom burden, disability, social isolation, financial insecurity, and HIV-related stigma and discrimination, indicating a need for comprehensive, evidence-based, people-centred healthcare models.
3.7. PROMs that capture information about symptoms should be incorporated into HIV clinical care to support patients’ involvement in their own care and to improve recognition of symptoms and problems that may have a negative impact on health and well-being, such as undiagnosed comorbidities or social issues.
Stigma and discrimination
4.1. HIV-related stigma and discrimination, including discriminatory laws as well as the social environment fostered by these laws, constitute major barriers to the successful implementation and uptake of comprehensive care models for PLHIV.
4.2 Negative consequences of HIV-related stigma and discrimination include reluctance to use health services, medication non-adherence, internalised stigma, depression, emotional distress, social exclusion, and poor HRQoL.
4.3. Promoting the holistic well-being of PLHIV in clinical and community care settings requires efforts to identify specific ways in which stigma and discrimination affect PLHIV and to respond with interventions at the service delivery, health system and structural levels.
4.4. Effectively countering HIV-related stigma and discrimination requires actions to address its intersectional nature. This means taking into account how HIV status and HIV risk intersect with other factors that may elicit stigma and discrimination, such as age, sexual orientation, gender identity, sex characteristics, race, religion, ethnicity, indigenous status, national origin, migrant status, drug use, disability, incarceration, and sex work.
4.5. HIV-related stigma and discrimination are consistently reported in healthcare settings worldwide and present major barriers to service uptake, service delivery, and retention in care, including for non-HIV-specific health needs. This limits the effectiveness of integrated service delivery models that are essential for advancing the overall health and well-being of PLHIV.
4.6. Countering HIV-related stigma and discrimination in healthcare settings requires expanding the evidence base regarding how to effectively address the root causes of these problems and scaling up interventions shown to achieve lasting improvements.
4.7. All types of healthcare settings should provide patients with information about their rights and should have formal, confidential channels for reporting stigmatising and discriminatory behaviours and experiences. There should also be mechanisms for redress when violations of human rights have occurred.
4.8. Validated instruments should be utilised to monitor progress toward the achievement of global and national HIV-related stigma and discrimination targets.







